Essential & Black: A 28-Year-Old Kenyan Nurse Who Insists That Nurses Are Humans Too
"...I put my personal care needs aside — whether it be a bathroom break, water break, or lunch break — to make sure that everyone is receiving the best care I can give at this time."
Speak Patrice Presents: Coronavirus News for Black Folks is an independent newsletter that aims to empower our community by sharing coronavirus (COVID-19) news and stories as they relate to the Black Diaspora.
Please consider (1) clicking that itty bitty ❤️at the top of this email next to my name to “like” us, (2) subscribing, and (3) supporting this newsletter by sharing it with friends and family.

Illustration by Christina Bauer for Coronavirus News for Black Folks
Who: Yunuke Bosire, a 28-year-old Kenyan woman who lives in Jersey City, New Jersey.
Essential job: She’s a registered nurse with 24/7 Nurses Agency.
Location: As an agency nurse, Yunuke travels to and works at various facilities in the Tri-State region of New York, New Jersey, and Connecticut.
Work schedule: She leaves for work at 6:15 AM and her workday usually ends anytime between 7:45 to 9:00 PM. Her shifts are supposed to be 12 hours-long but often end up lasting 14 to 16 hours. She works 36 to 40 hours a week.
“As a primary nurse, my role is vast, especially during these times.
I must ensure that all my patients are cleaned, fed, and medicated. Some require require medication administered through feeding tubes, which can take at least 30-plus minutes per patient. I also check all of the patients’ oxygenation levels. If the levels are too low, they become hypoxic (editor’s note: an absence of enough oxygen in the tissues to sustain bodily functions), and if the levels are too high, they risk becoming dependent on outside oxygenation.
Then there’s the documentation. I must document everything that I do for every patient — every time I reposition them, change a dressing, place a new IV — all while wearing a head-to-toe bunny suit for protection. I also have to call and update patients’ family members, sometimes multiple times a day, as they are not allowed to be in the hospital. I like to FaceTime families, if possible, to give them visual updates as this is the closest thing we have to an actual in-person visit at this time.
While all of this is happening, I’m still receiving new orders from doctors, changing and adding medication, fluids, and changing care plans. These orders must be carried out in a timely manner, so I put my personal care needs aside — whether it be a bathroom break, water break, or lunch break — to make sure that everyone is receiving the best care I can give at this time.”
“I don’t know what each work shift will be like, so I always feel a great deal of anxiety.
Will today be the day I get exposed and fall ill? How many of the people I care for today will die despite the lengths I go to to try and keep them alive? How will I talk to family members in a respectful, hopeful manner even though I think their family member won’t make it through my shift today?
Also, about nine of my close colleagues have tested positive for COVID-19 and had to be out sick. Some are back, while others are still out sick for over a month now. This feeds my anxiety because I've been working so close to them. How have I been spared? Why I haven't fallen ill? If I were to get tested now, would it be positive?
These questions perpetuate my fears and keep me on high alert all the time. But I have to compartmentalize all of this because I need to be 100% prepared and present while caring for my other patients. That includes worrying about cross exposure (exposing one patient to another) and reviewing the donning and doffing (editors note: the putting on and taking off) of PPE every morning before entering work to make sure process is truly fresh in my head.”
“My chances of being infected with COVID-19 are so astronomical, I’m not sure I can even quantify them.
I work 36 to 40 hours a week with direct contact with positive COVID-19 patients, having to use the same N-95 mask and bunny suit for at least half of the shift. The only time we receive a replacement mask is if we’ve worn it for 8 hours straight or if it was damaged.
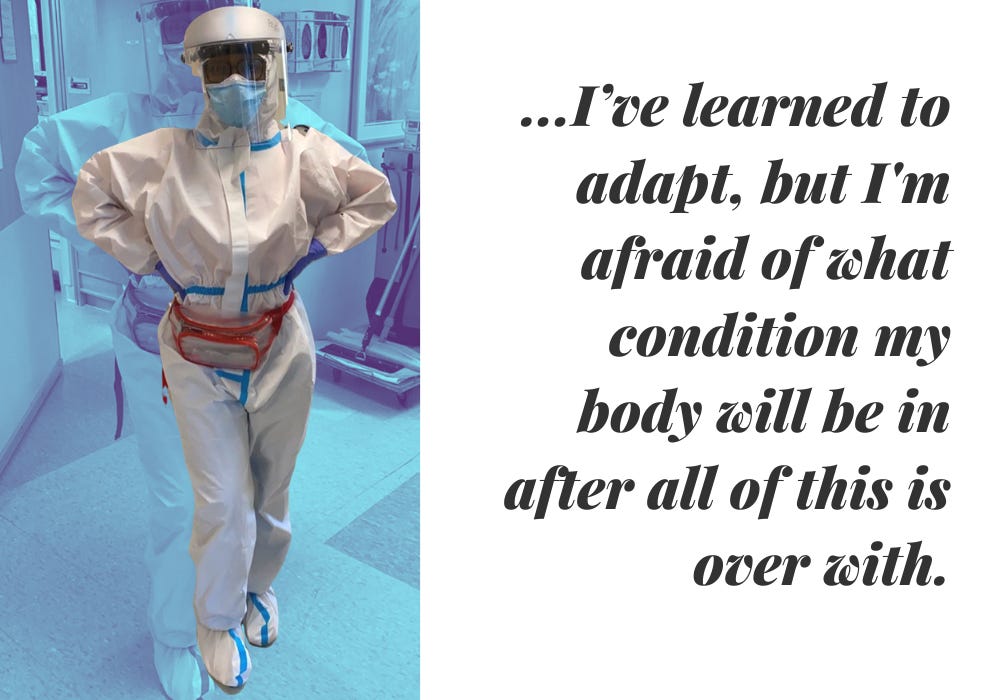
Wearing the PPE while carrying out my nursing duties is one of the most difficult things I’ve endured in my lifetime. Anyone who’s worn that mask knows it’s extremely difficult to breathe in. Between sweating all the time and not eating much at work, I’ve lost about 15 pounds since the pandemic began. Moreover, my colleagues and I don't drink enough water because using the bathroom means removing the entire suit and that increases the risk of contamination. And we don’t take breaks as much as usual because we have to doff (editor’s note: remove PPE) to go into the break room and we are only allowed to use two suits and masks for a 12 to 14 hour shift.
So I’ve learned to adapt, but I'm afraid of what condition my body will be in after all of this is over with.”
“My job demands every ounce of myself.
Nurses have the most interactions with patients out of any person in the hospital setting. So our attitude and demeanor can really affect our patients' outcomes. Even at our lowest moments, we must still be brave and do what is best for the patient.
One of the things I’ve found most difficult throughout this pandemic is the number of deaths I've seen. Despite being down, I have to muster an energetic, hopeful, and loving energy because I still have to care for other patients. I cannot bring that sad energy outside the room because that can have lasting effects on the next patient.
But I think that many people forget that nurses are humans too. We still feel sadness. We still cry. And yet we are still expected to rise up above all those emotions, almost immediately, to care for the next person. This is extremely hard.”

“My two biggest fears about COVID-19 are…
…that we know little about how this disease works so we cannot know if the treatment we are providing is the best and that we do not know what long term effect it will have on anyone that has been exposed.
This disease follows no normal pathology, and therefore it remains sort of a mystery. Each day we discover something new about the disease. At first it was said to not affect children, but now it is suspected to be triggering organ failure in children. Therefore, it is difficult to maintain hope and it almost feels like there is no true ending in site.
What will be the new normal after COVID-19? I’m not sure, but I fear we’ll be dealing with the ramifications of this disease for a long time and that it will affect the current treatment of chronic conditions.”
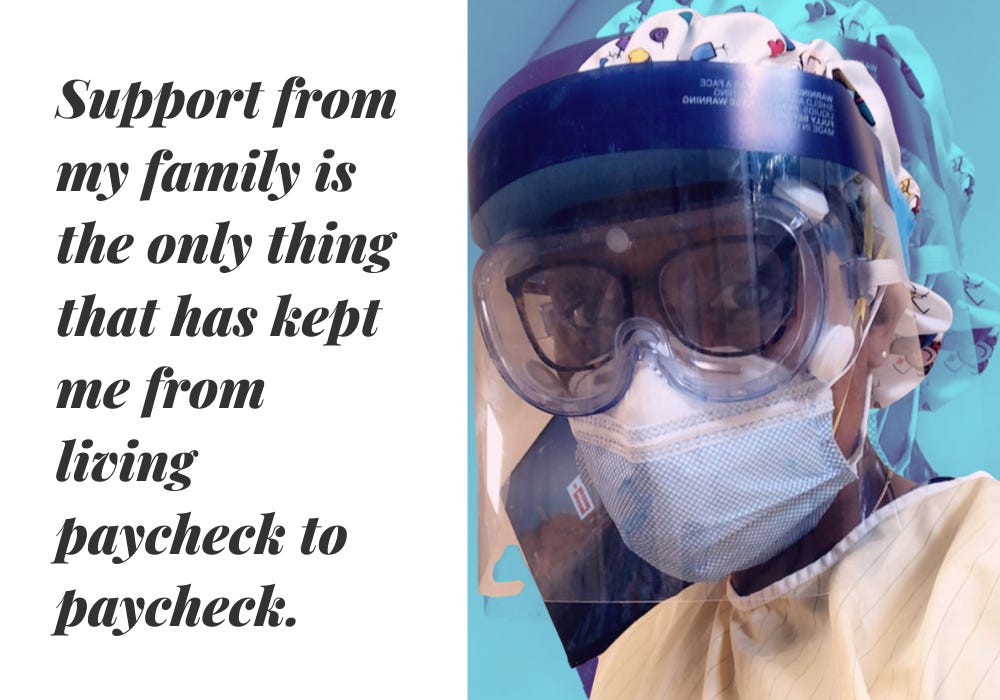
“Nurses are significantly underpaid. Support from my family is the only thing that has kept me from living paycheck to paycheck.
As nurses, we work so hard to get to where we are and then we are shortchanged, even through this pandemic. Then there’s the crappy insurance that deters me from wanting to even go to see my primary doctors. I find it appalling that, as a single person, I have to pay about $400 monthly for insurance that sends me a bill for $500 for a regular doctors visit.”
“Being a black agency nurse has been my life's greatest gift and challenge.
Staff nurses work day in and day out with the same rotation of nurses, doctors, techs and, in doing so, establish relationships and reputations over time. However, as an agency nurse, I bounce from facility to facility, filling in gaps and interacting with different people more frequently than any staff nurse would.
To put this all into perspective, staff nurses usually go through a two-week orientation period followed by a unit orientation for at least three weeks. I, on the other hand, have one day to learn the computer charting system, and one day, if that, to learn the unit setup.
And being Black adds another element to the equation because whenever I go to a new facility, I must prove that I am knowledgeable and can adapt quickly. I ALWAYS have to be my best. Because if I slip up or make a mistake, I'll be fulfilling not only agency nurse stereotypes, but racial stereotypes too. So I’ve learned to be meticulous with my documentation and how to read in between certain professional lines. I work so hard that I become irreplaceable, even as my environment regards me as disposable.”
“When I became a nurse, I made an oath to care for the sick — even during a pandemic.
I was trained to care for the sick and I love doing it, so I thank God that I’m healthy and can wake up daily, put on my bunny suit, and nurse someone back to health. The most rewarding experiences for me have been seeing some of my sickest patient leave the hospital and go home to fully recover. There are no words to truly describe that feeling. In those moments, I think to myself, ‘Wow! I helped that person get here.’ That’s what makes this all worthwhile and gives me hope that all the others still in the hospital bed will make it out too.”
“I know that nurses have been receiving much thanks from everyone, but I just want everyone to know that this is really a team effort.
There are social workers, physical therapists, respiratory therapists, and many more professionals who help nurses do our jobs and they deserve the same recognition. I hope that people gain a greater respect for healthcare providers as a whole and a better understanding of what goes into caring for extremely sick patients.”
This interview has been edited and condensed for clarity and length.
MORE ESSENTIAL & BLACK:
A Pregnant Hospital Worker in Delaware Who Prefers Work to Home But Feels Invisible
A Security Guard in Harlem, NY Who Feels Betrayed By Her Employer
A Pharmacy Technician In Rochester, NY Who Lives Paycheck to Paycheck
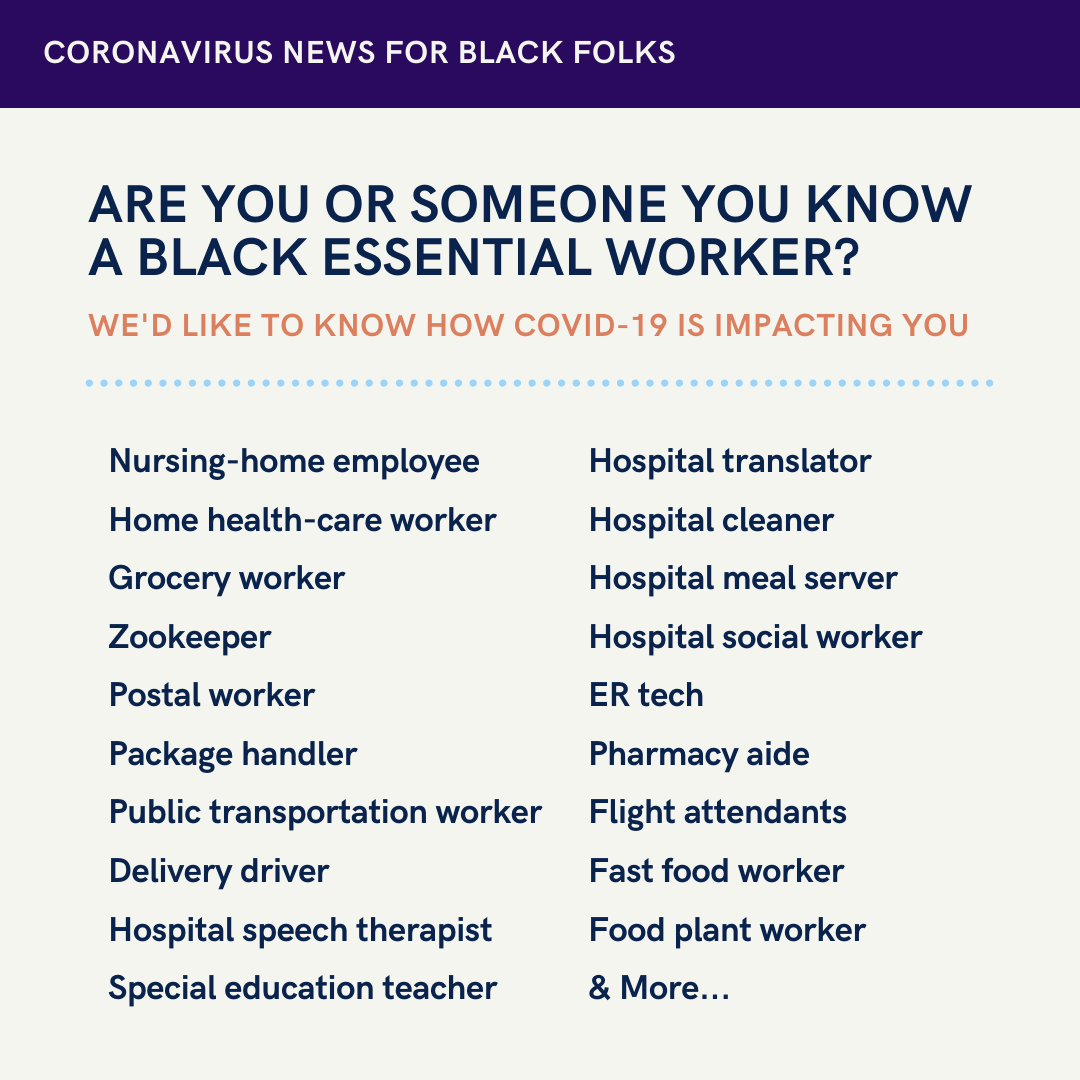
We want to share your COVID-19 pandemic experiences:
Are you a Black essential worker? Are you on the front line of the pandemic? Would you like to share your story for a potential feature in the newsletter?
Submit your story here: https://forms.gle/UTGTD9i9mXG1oNwY6
Not an essential worker? We still want to hear from you! Do you have an interesting story to tell about life during the pandemic?
Submit your story here: https://forms.gle/ygicBGtUYPrnJRUL7
WYD?
United States folks: What will you be doing this coming Memorial Day weekend? Working? Being still? Spending time with loved ones? All, some, or none of the above? (Did you even remember this was a holiday weekend? Because if you didn’t, I don’t blame you!) How about our international subscribers? Whatever you all end up doing (or not doing), I wish you good health.
I’ll be doing all of the above, including working on an op-ed for a publication that has to do with my work here at Coronavirus News for Black Folks. Peace out for now!
Stay safe and take care ✊🏿💗




